Dr. Poy is a senior scientist and a member of the Johns Hopkins All Children’s Institute for Fundamental Biomedical Research. He also is an associate professor of medicine and biological chemistry in the Johns Hopkins University School of Medicine. He studies the function of non-coding RNAs in energy metabolism and their regulatory role in the pathogenesis of obesity and diabetes.
Dr. Poy is among the first to describe how microRNA—tiny molecules that fine-tune how genes carry out the information encoded in our DNA—could target a specific gene and control insulin secretion. He is at the leading edge of microRNA research, which holds promise for understanding how these molecules contribute to an adaptive, compensatory response in the regulation of glucose homeostasis, and may be applied to treatment for diabetes and potentially other metabolic-based diseases related to the pancreas, heart and liver.
Born in Bethesda, Maryland, Dr. Poy studied biology and earned a Ph.D. in biomedical sciences at the Medical College of Ohio in Toledo. He did post-doctoral work with Markus Stoffel, M.D., Ph.D., at Rockefeller University and relocated in 2007 with Dr. Stoffel to the ETH-Zürich in Switzerland. In 2008, Dr. Poy started a 10-year stint at the Max Delbruck Center for Molecular Medicine in Berlin, Germany, before joining Johns Hopkins All Children’s in 2018.
Research
PITPNA in pancreatic beta-cell dysfunction and diabetes pathogenesis.
Critical to successful innovation in treating diabetes is the development of strategies for promoting insulin release and preventing pancreatic beta-cell destruction. Recent studies have highlighted defects in insulin processing and granule maturation that are linked to all major forms of diabetes; however significant conceptual gaps remain in our fundamental understanding of the causes of beta-cell dysfunction. The chronic demand for insulin production that occurs during insulin resistance and ultimately hyperglycemia can exacerbate cell dysfunction. This is compounded by ER and oxidative stress within the beta-cell that leads to cell death and loss of insulin production.
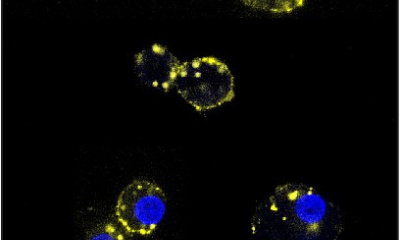
We previously identified miR-375 as the most abundant microRNA in the pancreatic beta-cell and established it as a potent regulator of insulin secretion; however, its most significant targets mediating beta-cell function remain to be determined. Here we establish Phosphatidylinositol transfer protein alpha (referred to as human PITPNA and mouse Pitpna), as a major target of miR-375 and regulator of insulin secretion. PITPNA shuttles phosphatidylinositol (PI) from the endoplasmic reticulum (ER) to the trans-Golgi network (TGN) for conversion to phosphatidylinositol-4 phosphate (PtdIns-4-P), an abundant membrane phospholipid previously shown to mediate insulin granule docking and mitochondrial dynamics. Our preliminary data shows 1) PITPNA is decreased in beta-cells of T2D human subjects, 2) reduction of PITPNA in human islets lowered cellular PI4-P levels and insulin granule maturation in addition to incurring accumulation of PI, and 3) conditional beta-cell specific deletion of Pitpna in mice (Ins-Cre; Pitpnaflox/flox) results in decreased insulin secretion and beta-cell mass, random-fed hyperglycemia, and increased expression of ER stress proteins. In this project, we hypothesize that decreased PITPNA in beta-cells during T2D reduces presentation of PI to PI4-K in the TGN thereby lowering subcellular distribution of PI4-P and disrupting insulin granule maturation. Moreover, we propose reduced PI shuttling leads to its accumulation in the ER impairing insulin processing, inducing ER stress and ultimately cell death. The goals of this study are: to delineate how decreased PITPNA causes beta-cell dysfunction; to restore PITPNA levels to normal in T2D human islets in an attempt to rescue insulin production, granule maturation, and secretion, and to lower expression of ER stress proteins.
These studies will determine how alterations in distribution of phospholipids, PI and PI4-P, is regulated by PITPNA and contributes to beta-cell dysfunction during T2D. We expect decreased PITPNA as a central factor controlling PI to PI4-P conversion. Thus, loss of PITPNA impairs insulin granule maturation and provokes ER stress. Completion of these studies will illustrate that regulation of PITPNA function is a novel therapeutic strategy for promoting insulin production and secretion as well as reversing beta-cell failure in major forms of diabetes.
CADM1 in Type 1 diabetes pathogenesis.
Type 1 diabetes (T1D) is characterized by the hyperglycemia resulting from autoimmune destruction of insulin-expressing beta-cells of the pancreas. No cure exists for this disease and despite progress in understanding islet pathology during T1D, key conceptual gaps still remain in identifying mechanisms that instigate immune cell infiltration and their recognition of beta cells. Given the established role of autoreactive T-cells in mediating beta-cell destruction during T1D, continued emphasis remains on identifying the islet proteins that mediate immune cell infiltration that could potentially be targeted to both preserve pancreatic beta-cell mass, and prevent the immune response that initiates T1D pathogenesis.
Our previous work showed increased expression of the gene CADM1 (referred to as human CADM1 and mouse Cadm1) in myeloid cells within the pancreatic islets of auto-antibody positive (aAb+) and in T1D human subjects. As a cell membrane surface protein, CADM1 mediates interaction between different cell types including immune cells and endocrine cells. Notably, Cadm1 (also known as Necl2) has been shown to act as a ligand for the receptor CRTAM (Class I–restricted T cell–associated molecule) present in CD8+ T-cells, a cell population widely known to infiltrate the pancreas and facilitate pancreatic beta-cell destruction during T1D. Here we hypothesize increased levels of CADM1 in endocrine cells and macrophages within the pancreatic islet facilitate recruitment of cytotoxic CD8+ T-cell populations. Our preliminary results show that treatment with a monoclonal ‘neutralizing’ antibody raised against CADM1 attenuates onset of autoimmune diabetes in mice. This project will elucidate the changes in the immune cell repertoire of the pancreas resulting from this antibody treatment during the pre-symptomatic phase of the disease. In this study we will ascertain how the CADM1 antibody affects T and B cell activation and whether there is a critical window for antibody treatment before disease onset to suppress the autoimmune attack on the pancreas. Successful outcomes of these preclinical studies will lay the foundation for the development of humanized CADM1 ‘neutralizing’ antibodies each targeting unique parts of the extracellular domain that could constitute an optimal strategy for preventing or potentially treating and curing individuals with T1D.
Cadm1 regulation of body weight and energy homeostasis.
Obesity induces activation of the innate immune system and macrophages have been shown to play a critical role in the chronic inflammation that underlies adipose tissue dysfunction. Sympathetic innervation of adipose tissue promotes lipolysis and the reduction of adiposity through norepinephrine (NE) signaling, and recent studies have demonstrated the role of sympathetic neuron-associated macrophages (SAMs) in mediating catecholamine clearance and degradation. Identification of these specific interactions within white and brown adipose tissue (WAT and BAT, respectively) in humans has provoked interest for their potential role as a target for pharmacological intervention to counter obesity and its co-morbidities. Despite these advances, conceptual gaps remain in terms of identifying the molecular mechanisms that mediate neuronal-immune cell interactions directing sympathetic neuronal activity, lipolysis, and adaptive thermogenesis.
Recent genome–wide association studies have identified an association between body mass index (BMI) and a locus near Cell Adhesion Molecule1 (referred to as human CADM1 and mouse Cadm1), which encodes a membrane protein mediating homotypic intercellular contact between immune and neuronal cells. We have previously shown that this risk variant correlates with increased hypothalamic CADM1 expression in human subjects and inducing neuronal Cadm1 expression promoted weight gain and insulin resistance in mice. While we established neuronal Cadm1 in regulating body weight, energy expenditure, and adaptive thermogenesis, increased numbers of Cadm1-expressing macrophages were observed in WAT after high fat diet feeding suggesting Cadm1 may mediate increased binding of SAMs with sympathetic fibers in adipose tissue. To test this hypothesis, we developed conditional mutant mice where Cadm1 expression is absent in cells of the myeloid lineage including mature macrophages. Our initial results show that Cadm1-deficient mice exhibit reduced body weight, and increased energy expenditure and insulin sensitivity. We expect to establish Cadm1 blocking antibodies as a potential therapeutic strategy for improving pre-diabetic complications including obesity, insulin resistance, and glucose intolerance. Future clinical strategies may leverage CADM1 SNP data with CADM1 blocking antibodies as a ‘precision medicine’ approach for averting obesity and its co-morbidities.


Selected Publications
- Yeh YT, Sona C, Yan X, Pathak A, McDermott MI, Xie Z, Liu L, Arunagiri A, Wang Y, Cazenave-Gaussiot A, Ghosh A, von Meyenn F, Najjar SM, Jia S, Traynor-Kaplan A, Arvan P, Barg S, Bankaitis VA, and Poy MN. Restoration of PITPNA in Type 2 diabetic human islets reverses pancreatic beta-cell dysfunction. Nature Communications. 2023 Jul 17;14(1):4250. doi: https://doi.org/10.1038/s41467-023-39978-1.
- Nimptsch K, Aydin EE, Chavarria R, Janke J, Poy MN, Oxvig C, Steinbrecher A, Pischon T. Pregnancy associated plasma protein-A2 (PAPP-A2) and stanniocalcin-2 (STC2) but not PAPP-A are associated with circulating total IGF-1 in a human adult population. Scientific Reports. 2024 Jan 20;14(1):1770. doi: 10.1038/s41598-024-52074-8. (Conceptual input, manuscript and data analysis)
- Kasinathan D, Guo Z, Sarver DC, Wong GW, Yun S, Michels AW, Yu L, Sona C, Poy MN, Golson ML, Fu D. Cell-surface ZnT8 antibody prevents and reverses autoimmune diabetes in mice. Diabetes. 2024 Feb 22:db230568. doi: 10.2337/db23-0568. (Performed experiments, manuscript editing and data analysis)
- Sona C, Yeh YT, Li Y, Liu X, Ghosh A, Hinte LC, Ku MC, Rathjen T, Niendorf T, Yu G, Jia S, Kononenko NL, Luo J, Lin J, von Meyenn F, Yan X, and Poy MN. Glutamatergic Argonaute2 regulates formation of the neurovascular unit in mice. (In Press at Science Signaling)